Where is your tongue “parked”?
Let’s talk about where your tongue is “parked” or resting whenever you are not talking or eating. Our tongue should “live” in the roof of our mouth, nestled between our teeth. This means your tongue tip is on the incisive papilla (those bumps right behind your top middle teeth) and the middle and back of your tongue is resting on the roof of your mouth.
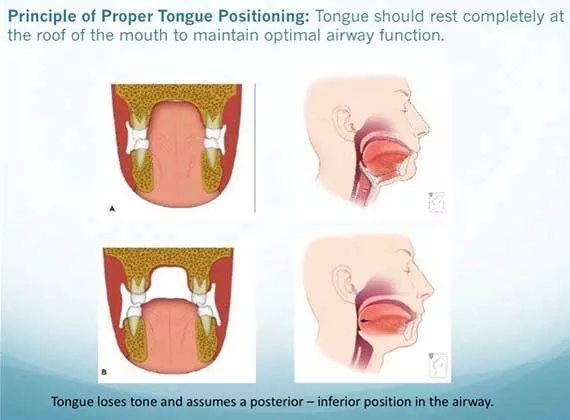
This position allows for optimal palatal, upper and lower jaw growth and development, it also allows for easy and natural nasal breathing (which we will talk about the benefits in another post). Our tongue acts as a natural “palatal expander” and allows the maxillary dental arch to form in a flat, U-shape vs. a high arched palate.
When our tongue is resting low and fronted in our mouth, the palate starts to form into a high/vaulted and narrow shape. It’s important to remember that the floor of our nasal cavity is the roof of our mouth. Therefore, if our palate is vaulted and high it may impact the ability to easily breathe through our nose. A low and fronted tongue also can affect dentition and your bite.
This is why our office works SO closely with our local airway-centric dentists and Ear Nose and Throat doctor. We are in close collaboration with both offices because what we do in the orofacial myology realm overlaps so much. Our local airway centric pediatric dentist will typically screen children and identify any suspected tethered oral tissue ties (aka tongue, lip or cheek ties), high/narrow palate or potential airway concerns. The children then are referred to us to complete a comprehensive orofacial myology assessment where we assess function (see Orofacial MyoWHAT?!?). We work with the dentist to determine an individualized plan regarding myofunctional therapy, if a release is needed and when and if appropriate to start palatal expansion. Palatal expansion is an important part of the myo puzzle because there has to be room for that tongue to rest on the roof of the mouth.
Why do we work with an ENT doctor? In our assessment if we find that the patient is primarily breathing through their mouth we need to figure out if it’s possible for the person to breathe through their nose. It may be difficult due to enlarged tonsils, adenoids or nasal obstructions so we refer to an ENT to assess the patient’s airway, typically prior to starting myofunctional therapy. Once the airway is “cleared” and it’s determined there is no obstruction then we get to work at establishing a new oral “habit” where we have to re-teach the tongue where to rest. This is done through weekly therapy and daily “homework” and can be completed in 6 months if we have a motivated patient!