10 Holiday Gift Guide Ideas (Speech and OT Therapist Approved!) 2024 Edition
The holiday season is a great time to find gifts that are not only fun but also help our little ones learn and grow. Toys and activities that encourage communication, language development, and motor skills, along with allowing young children to explore the sensory system can make a big impact. At this stage, kids are learning to express themselves and understand the world around them, so gifts that build on those skills are a perfect choice. Whether it’s an interactive storybook or a simple musical instrument, these kinds of simple gifts make learning feel like play. Plus, they’re a great way for parents and kids to connect while introducing important skills like communication and vocabulary. It can be difficult to decide which gifts to buy out of the many available. We compiled a short list of our favorite toys and games that we like to use in speech and occupational therapy and at home with our children!
1. Interactive Storybooks (Ages 0+)
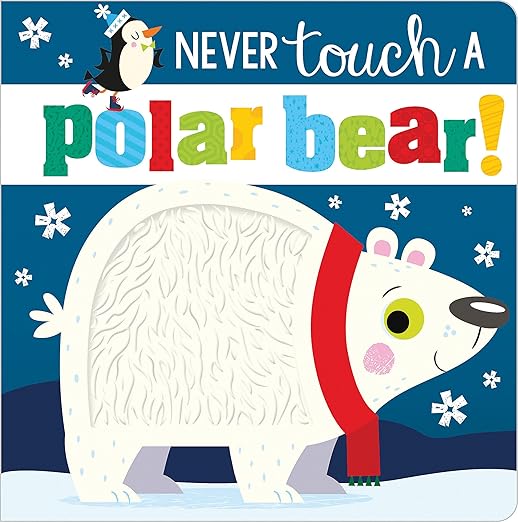
These books have something to touch and feel on every page encouraging early interaction with books, and there is a book for every season or a book to fit every season.
Language goals/core vocabulary to incorporate: “animal, monster, or dinosaur noises (moo, baa, roar), touch + X, more, turn the page”
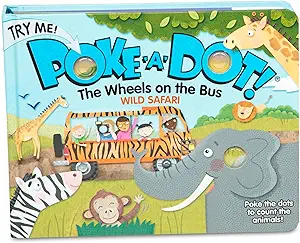
Encourage interaction on every page engaging early readers while targeting fine motor skills.
Language goals/core vocabulary to incorporate: “animal noises, push, more/all done”
2. Laugh and Learn Smart Stages Piggy Bank (Ages 1+)

Language goals/core vocabulary to incorporate: “open/close, nose, in/out”
Target fine motor skills and hand/eye coordination.
3. Musical Instruments (Ages 1+ supervised)

Simple instruments like tambourines, maracas, or xylophones encourage exploration of sounds and rhythms, aiding in listening skills.
Language goals/core vocabulary to incorporate: “bang, shake, more, nursery rhymes.”
Target fine motor skills.
4. Rainbow Spinning/Stacking toy (Ages 6 months+)

Language goals/core vocabulary to incorporate: “on/off, ready, set, GO!, more, down, colors.”
Target spatial concepts and motor skills.
5. Critter Clinic (Ages 2+)

Language goals/core vocabulary to incorporate: “open/close, Ouch, uh-oh, help + animal, animal sounds (meow, woof,) animal names.”
Target spatial concepts and imaginative play.
6. Vehicle sound puzzle (Ages 1+)
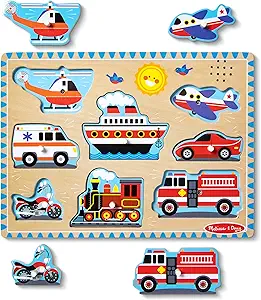
Language goals/core vocabulary to incorporate: “on/off, vroom, Whee-oo, chugga-chugga-choo-choo, ship, train, more.”
Targets fine motor skills: pincer grasp.
7. Hahahaland 2-in-1 Car and Ball Toy (Ages 1+)

Language goals/core vocabulary to incorporate: “colors, my turn/your turn, down, bang, hit + color, vroom”
8. Little Tikes First Slip and Slide (Ages 1+)

Sometimes it takes a little movement to get children vocalizing!
Language goals/core vocabulary to incorporate: “Ready, set, GO!, up/down, slide, more, whee,”
Target gross motor skills, balance and coordination, spatial awareness, and vestibular stimulation.
9. Melissa and Doug Food Cutting Play Set (Ages 2+)

Language goals/core vocabulary to incorporate: “cut + food, yum, yuck, eat, counting, I want + food.”
Target fine motor skills.
10. Tongues Out! (Ages 4+)
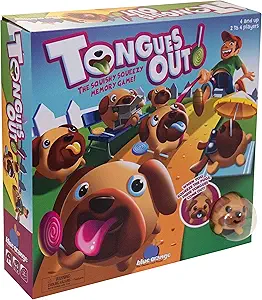
Language goals to increase core vocabulary: “Find + color, not + color.”
Target motor skills, social communication (taking turns), and negation (not blue).