OT Month: What Are Primitive Reflexes—And Why Integration Matters for Your Child's Development
By Kaysie Smith, MSOTR/L, CLC
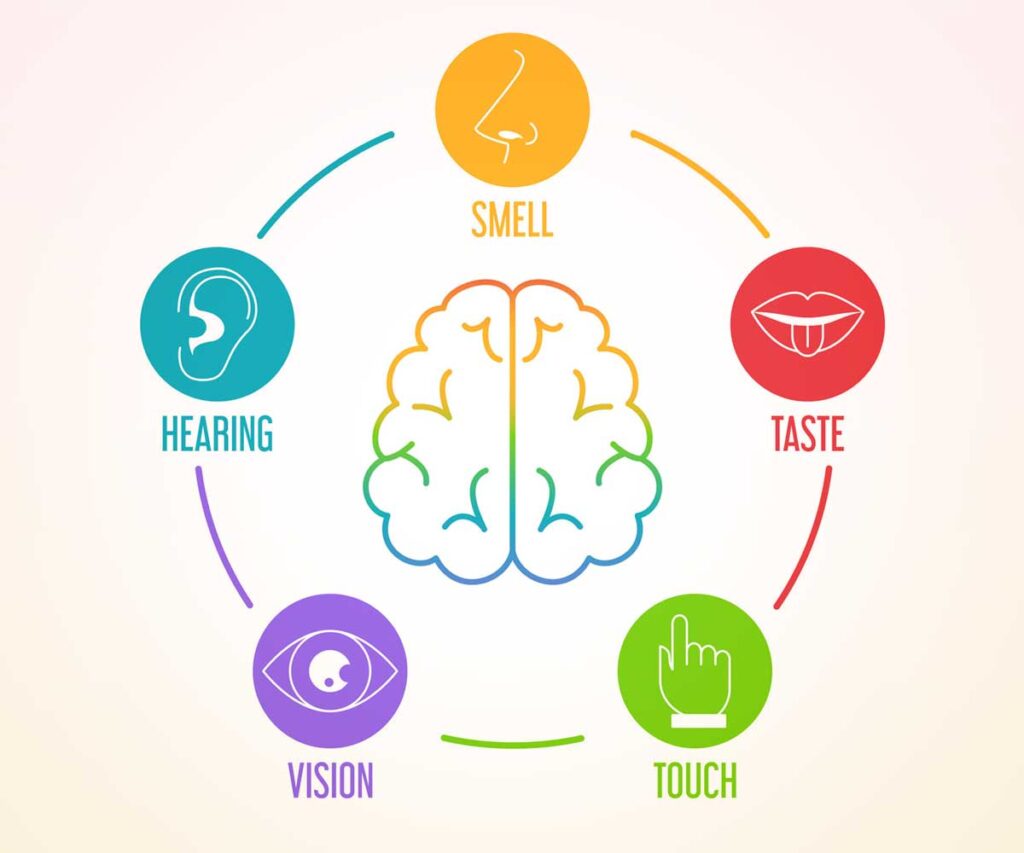
From the moment your child is born, their brain is busy wiring up the skills they’ll need to thrive—starting with reflexes that help them navigate the world. Primitive reflexes are automatic, involuntary movements that babies are born with. They’re essential for survival and early development—but here’s the key: they’re supposed to disappear, or "integrate," as a child grows. When these reflexes stick around longer than they should, they can interfere with motor coordination, sensory processing, attention, and even emotional regulation.

What Are Primitive Reflexes?
Primitive reflexes are the brainstem-driven movements we all start life with. For example:
- Moro reflex: Also called the startle reflex, where a baby flings their arms out and then curls in.
- ATNR (Asymmetrical Tonic Neck Reflex): When a baby turns their head to one side, the arm on that side extends.
- STNR (Symmetrical Tonic Neck Reflex): Helps babies get up on hands and knees for crawling.
- Palmar grasp, rooting, spinal galant—the list goes on.
These reflexes help babies learn to move, interact with their environment, and develop postural control. But they should naturally integrate as the brain matures—usually within the first year of life.
What Happens If Reflexes Don’t Integrate?
If a child retains primitive reflexes beyond the typical age, they may experience:
- Poor coordination or balance
- Difficulty sitting still or maintaining posture
- Trouble with handwriting or fine motor skills
- Delayed speech or language development
- Sensory sensitivities or emotional outbursts
- Challenges with reading, focus, or attention
For example, a retained ATNR can make it hard for a child to cross midline—an essential skill for reading and writing across a page. That child might tilt their head or move their whole body to track words, leading to fatigue and frustration in the classroom.
Why Reflex Integration Therapy Helps
Occupational therapists assess reflexes as part of a holistic developmental evaluation. If retained reflexes are present, we use neurodevelopmental movement-based exercises to help "repattern" the brain and support integration. These movements are purposeful and repetitive—essentially giving the nervous system a second chance to develop the way it was meant to. Over time, we see improvements in coordination, focus, emotional regulation, and overall confidence.
Signs Your Child Might Benefit from Reflex Integration Exercises
If your child:
- Tires easily when writing or doing homework
- Avoids climbing, riding a bike, or balancing
- Has strong emotional reactions or meltdowns
- Struggles with coordination or handwriting
- Appears clumsy or bumps into things frequently
…it may be worth scheduling a developmental occupational therapy evaluation.
Final Thoughts
Retained primitive reflexes are more common than you might think—but the good news is, with the right support, kids can catch up and thrive.
Early intervention can make a world of difference, and reflex integration is a powerful tool in helping children unlock their full potential—academically, socially, and emotionally. Specific movement patterns and play-based activities are used to support the nervous system and help integrate reflexes.
If you are curious about reflex integration, don’t hesitate to reach out to our team at Gro!




















 Childhood Apraxia of Speech- or CAS is a neurological pediatric speech sound disorder where the precision and consistency of movements underlying speech are impaired in the absence of neuromuscular deficits (i.e. abnormal reflexes or tone). CAS may occur as a result of a known neurological impairment (i.e. brain damage) or independently. Think of it this way: the child knows what they want to say but has trouble coordinating the precise movements of the articulators to get the message out.
Childhood Apraxia of Speech- or CAS is a neurological pediatric speech sound disorder where the precision and consistency of movements underlying speech are impaired in the absence of neuromuscular deficits (i.e. abnormal reflexes or tone). CAS may occur as a result of a known neurological impairment (i.e. brain damage) or independently. Think of it this way: the child knows what they want to say but has trouble coordinating the precise movements of the articulators to get the message out.
 Intellectual Disabilities- or ID is characterized by the onset in the developmental period (before age of 22 years), significant limitations in adaptive behavior and significant limitations in intellectual functioning. The diagnosis of an ID is not made by a speech pathologist but children with IDs may benefit from speech, language and/or auditory processing therapy to help improve functional communication in the child’s daily life.
Intellectual Disabilities- or ID is characterized by the onset in the developmental period (before age of 22 years), significant limitations in adaptive behavior and significant limitations in intellectual functioning. The diagnosis of an ID is not made by a speech pathologist but children with IDs may benefit from speech, language and/or auditory processing therapy to help improve functional communication in the child’s daily life.